Neuromodulation techniques for Alzheimer’s disease and age-related cognitive decline.
By Marom Bikson (City College of New York)
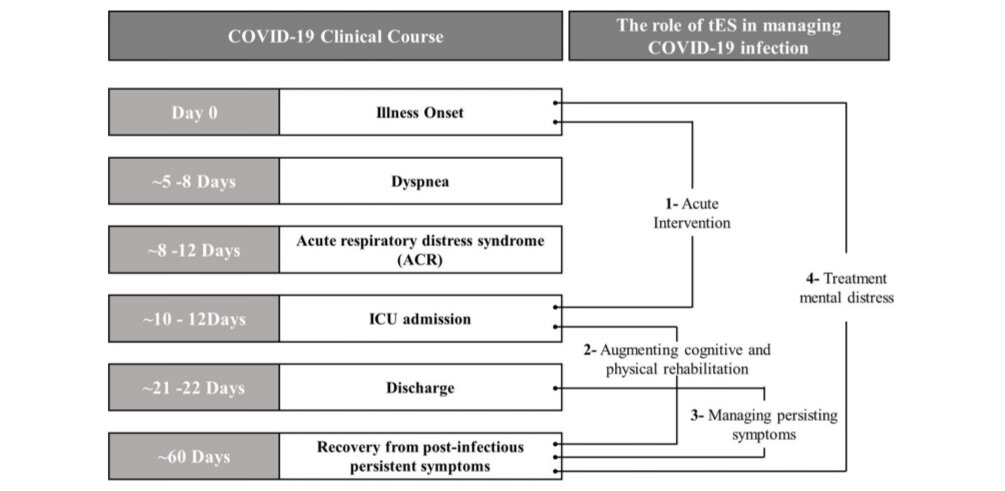
Even as the societal burden of Alzheimer’s disease and related dementias increases, pharmaceutical trials targeting the associated toxic protein aggregates have disappointed. Neuromodulation devices apply energy (eg, electrical or ultrasound) to the brain to promote the recovery of function. As an alternative to pharmacologic interventions (drug therapies), neuromodulation therapies are non-systemic and can directly target brain regions with stimulation waveforms designed to boost specific brain processes.
Neuromodulation devices can be surgically implanted or used non-invasively (on the scalp). Noninvasive neuromodulation treatments can involve repeated visits to a clinic, whereas some devices can be used at home. Neuromodulation therapies are established for indications such as depression, pain, epilepsy, and Parkinson’s disease, and include patients who were not responsive to drug therapies. Neuromodulation trials show promise in maintaining, and even reversing, cognitive decline in Alzheimer’s and related neurodegenerative disorders.
A neuromodulation technique using “shockwave” ultrasound received regulatory medical CE approval for use in Alzheimer’s disease and mild-to-moderate dementia. Patients who received this noninvasive, painless treatment at outpatient clinics over the course of six visits within 2 weeks showed neuropsychological improvements lasting at least 3 months. (1) Not to be confused with transcranial focused ultrasound stimulation, “shockwave” ultrasound applies isolated acoustic pulses that in turn enhance neurovascular function. (2)
A wearable neuromodulation technique called transcranial direct current stimulation (tDCS) is also actively trialed for Alzheimer’s and age-related cognitive decline. tDCS is suitable even for at-home use (it could be made available over the counter) and may provide unique therapeutic potency by “cleansing the brain.”
More plaques versus less clearance in Alzheimer’s disease: chicken and egg
A key question in Alzheimer’s disease research is: how much of the accumulation of toxic protein aggregates reflect abnormal production versus disrupted clearance mechanisms? (3) Therapeutically, this is a moot point unless we have treatments that can boost brain clearance.
Accumulation of toxic protein aggregates-amyloid-β (Aβ) plaques and hyperphosphorylated tau tangles is the pathologic hallmark of Alzheimer’s disease; however, drug trials targeting these proteins have been unsuccessful.
Because they remove cellular waste products and deliver nutrients to the interstitial space (the space around neurons), the clearance systems of the brain are critical for normal brain function. Brain interstitial fluid clearance systems become disrupted with Alzheimer’s disease progression.(4)
Interstitial fluid clearance mechanisms may also be generally compromised with age, which may further be linked to the role of clearance during sleep.(5,6)
How transcranial direct current stimulation works
Go with the (blood) flow
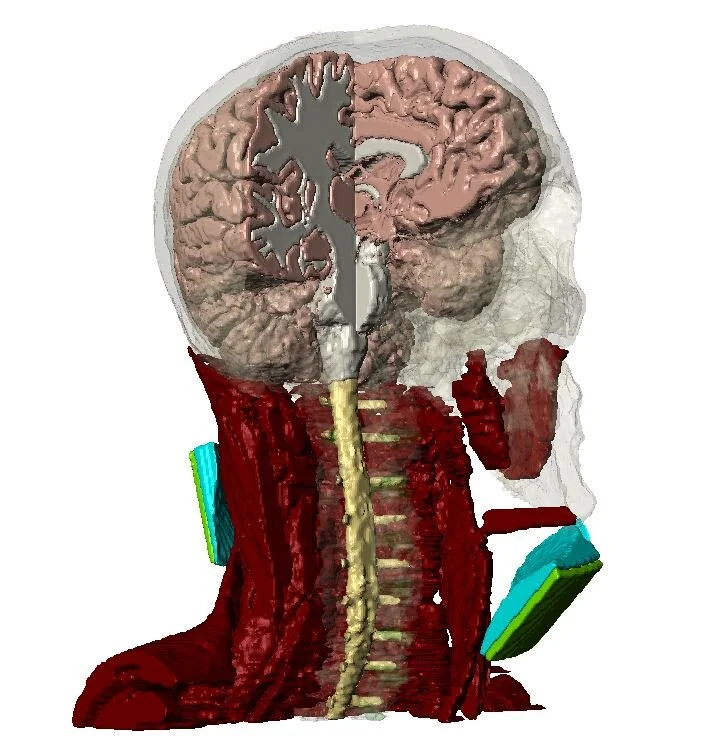
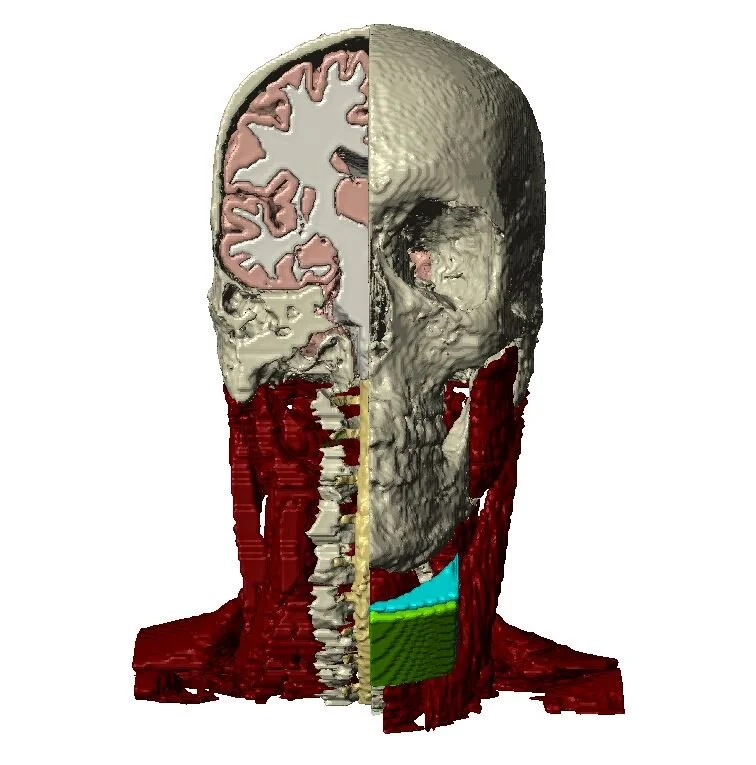
Transcranial direct current stimulation (tDCS) applies a low fixed-intensity (direct current) electrical current to the brain through electrodes placed on the scalp. Powered by a 9-volt battery, tDCS is painless, safe, and can be administered at home. (7,8)
Like most other treatments of brain disease, neurons are the de facto target of tDCS.
Adverse effects of tDCS are very mild, including tingling or itching sensations that resolve as stimulation ends, and skin reddening (erythema) that can persist a while longer. Given this sign of profound change in blood flow at the scalp by tDCS, one may ask: could changes in neurovascular function also be occurring?
In fact, there is extensive brain imaging data of the brain vascular response to tDCS. However, as is typically the case with brain imaging techniques that rely on hemodynamic response (eg, blood-oxygen-level-dependent imaging functional MRI), this vascular response is considered an epiphenomenon, which means the detection of vascular action is presumed to be secondary to neuronal stimulation.
This makes sense based on the underlying principle of neurovascular coupling: cerebral blood supply is increased in response to neuronal metabolic activity, as well as to remove toxic byproducts from the interstitial space. But could tDCS swap the regular order of neurovascular coupling: activating blood flow first, which then leads to secondary neuronal modulation? These questions are hard to answer, precisely because neuronal activity and brain vasculature are intimately linked. To convincingly show a primary vascular response, one would require a “brain” consisting of vasculature but no neurons.
Blood vessel walls, including those making up neuronal vasculature, are formed by endothelial cells, which are the barrier between the brain’s interstitial space and circulating blood. This blood–brain-barrier (BBB) is an exceptionally regulated barrier as a result of tight bonds between endothelial cells, known as tight junctions. Cultured endothelial cells on a filter form a BBB model, which can be absent of other cells types. Using such a model, we showed that direct current stimulation directly activates endothelial cells, thereby providing direct evidence of how brain vasculature could respond to tDCS. (9)
We showed that the neurovascular endothelial cells that make up the BBB are a direct cellular target of tDCS, which supports ongoing trials where activating brain blood flow can support recovery of function (eg, in acute stroke). (10)
Further analyses of the mechanism’s underlying BBB stimulation led us to a novel therapeutic pathway for Alzheimer’s disease: boosting brain clearance.
Flush and rinse
Direct current stimulation drove water transport across the BBB model through the mechanism of electro-osmosis, which occurs when electrical current flowing through a network of cells produces an associated drag on water. The smaller the gap between cells, the more electro-osmosis, and the BBB is exceptionally tight. Moreover, when the current flow is in a sustained direction, as is the case for tDCS, so is the water flow.
Along with water flow, we showed boosting of specific molecule transport and endothelial-cell gene activation. We reproduced our finding that tDCS boosts transport across the BBB in an intact animal model.(11)
We made a further striking discovery: in addition to enhancing transport across the BBB, tDCS also increased diffusivity within the brain interstitial space.(12)
Taken together, this indicates that tDCS, a noninvasive neuromodulation technique with minimal side effects, could boost brain clearance by both driving water across the BBB and enhancing transport around neurons.
Ongoing and future clinical trials: treating Alzheimer’s disease with tDCS
In patients with Alzheimer’s disease or age-related atypical cognitive impairment, clinical trials with tDCS treatment have been completed, and expanded trials are ongoing. The National Institutes of Health (NIH)-funded study Augmenting Cognitive Training in Older Adults (ACT) is a Phase 3, definitive, multi-site, randomized clinical trial of 360 older adults to establish the benefit of delivering tDCS to remediate age-related cognitive decline. (13)
The randomized controlled Prevention of Alzheimer’s dementia with Cognitive remediation plus tDCS in Mild cognitive impairment and Depression (PACt-MD) study includes 375 older participants with either atypical cognitive impairment and/or major depression.(14)
While most trials evaluate in-clinical treatment, an NIH-funded, randomized, double-blind trial study at Albert Einstein College of Medicine, Bronx, NY, will evaluate the effects of 6 months of at-home tDCS in 100 patients with mild-to-moderate Alzheimer's disease.(15)
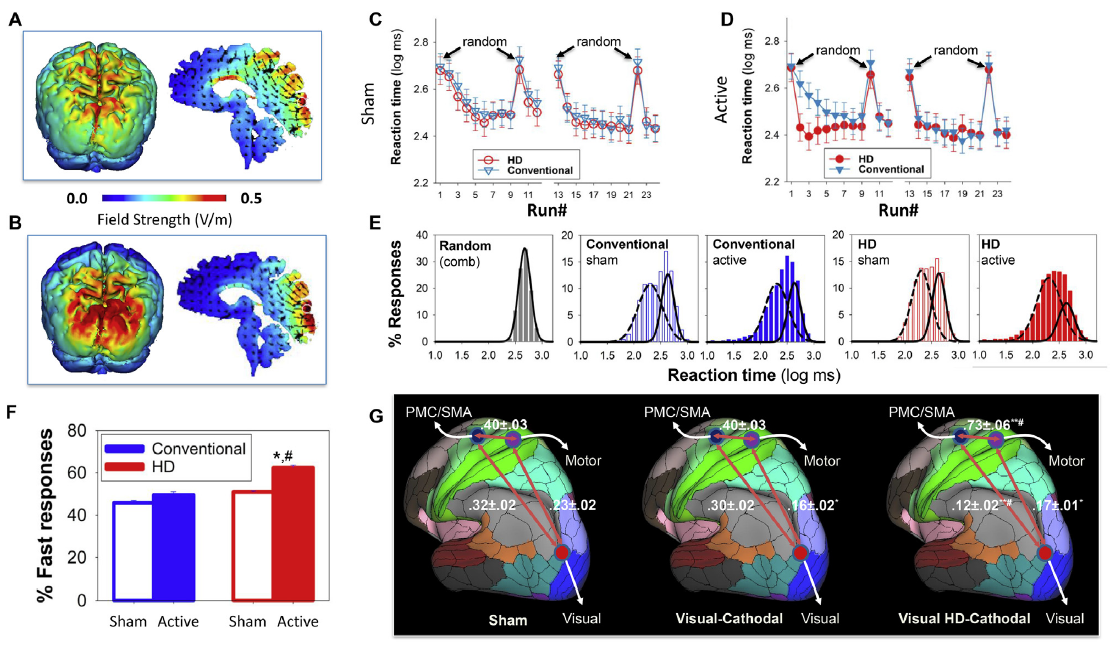
The Veterans Administration and NIH are supporting two double-blind, randomized, controlled trials in patients with mild cognitive impairment (146 patients) or Alzheimer’s disease (100 patients) using High-Definition tDCS, a form of tDCS that can focally target brain regions.(16,17)
These studies will further use imaging to evaluate changes in both cerebral blood and amyloid and tau plaque severity.
Clinical trials of tDCS around the world are recruiting hundreds more older adults with mild cognitive impairment, Alzheimer’s disease, and related dementia. These trials were founded on the established actions of tDCS on neurons, including promoting synaptic plasticity. But tDCS may also be boosting brain vascular function and driving brain clearance mechanisms. Even as definitive clinical data on the treatment of age-related cognitive decline continue to emerge, further work characterizing these special mechanisms of tDCS can be used to optimize therapies.
Key points
Neuromodulation devices are non-drug therapies designed to boost specific therapeutic mechanisms.
Transcranial direct current stimulation (tDCS) is a wearable device that is actively trialed for the treatment of Alzheimer’s disease and mild cognitive impairment.
In addition to stimulating neurons, tDCS enhances brain blood flow and clearance mechanisms.
The boosting of brain clearance mechanism by tDCS is a powerful mechanism to reverse the build-up of toxic proteins associated with Alzheimer’s disease.
References
Beisteiner R, Matt E, Fan C, et al. Transcranial pulse stimulation with ultrasound in Alzheimer's disease–a new navigated focal brain therapy. Adv Sci (Weinh). 2019;7:1902583.
Hatanaka K, Ito K, Shindo T, et al. Molecular mechanisms of the angiogenic effects of low-energy shock wave therapy: roles of mechanotransduction. Am J Physiol Cell Physiol. 2016;311:C378-385.
Tarasoff-Conway JM, Carare RO, Osorio L, et al. Clearance systems in the brain–implications for Alzheimer disease. Nat Rev Neurol. 2015;11:457-470.
Peng W, Achariyar TM, Li B, et al. Suppression of glymphatic fluid transport in a mouse model of Alzheimer's disease. Neurobiol Dis. 2016;93:215-225.
Kress BT, Iliff JJ, Xia M, Wang M, et al. Impairment of paravascular clearance pathways in the aging brain. Ann Neurol. 2014;76:845-861.
Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373-377.
Bikson M, Grossman P, Thomas C, et al. Safety of transcranial direct current stimulation: evidence based update 2016. Brain Stimul. 2016;9:641-661. PDF
Charvet LE, Kasschau M, Datta A, et al. Remotely-supervised transcranial direct current stimulation (tDCS) for clinical trials: guidelines for technology and protocols. Front Syst Neurosci. 2015;9:26.
Cancel LM, Arias K, Bikson M, Tarbell JM. Direct current stimulation of endothelial monolayers induces a transient and reversible increase in transport due to the electroosmotic effect. Sci Rep. 2018;8:9265. PDF
NCT03574038. Transcranial direct current stimulation as a neuroprotection in acute stroke (TESSERACT).https://clinicaltrials.gov/ct2/show/NCT03574038.Accessed November 28, 2020.
Shin DW, Fan J, Luu E, et al. In vivo modulation of the blood-brain barrier permeability by transcranial direct current stimulation (tDCS). Ann Biomed Eng. 2020;48:1256-1270.
Xia Y, Khalid W, Yin Z, Huang G, Bikson M, Fu BM. Modulation of solute diffusivity in brain tissue as a novel mechanism of transcranial direct current stimulation (tDCS). Sci Rep. 2020;10:18488.
NCT02851511. Augmenting cognitive training in older adults (ACT).https://clinicaltrials.gov/ct2/show/NCT02851511. Accessed November 28, 2020.
NCT02386670. Prevention of Alzheimer's disease with CR plus tDCS in mild cognitive impairment and depression (PACt-MD) (PACt-MD).https://www.clinicaltrials.gov/ct2/show/NCT02386670. Accessed November 28, 2020.
NCT04404153. NeurostImulation for cognitive enhancement in Alzheimer's disease (NICE-AD).https://clinicaltrials.gov/ct2/show/NCT04404153. Accessed November 28, 2020.
NCT02155946. Promoting adaptive neuroplasticity in mild cognitive impairment.https://clinicaltrials.gov/ct2/show/NCT02155946. Accessed November 28, 2020.
NCT03875326. Stimulation to improve memory (STIM).https://clinicaltrials.gov/ct2/show/NCT03875326. Accessed November 28, 2020.