Gebodh, N., Esmaeilpour, Z., Adair, D., Chelette, K., Dmochowski, J., Woods, A. J., Kappenman, E. S., Parra L. C., Bikson M. (2019). Inherent physiological artifacts in EEG during tDCS. NeuroImage, 185, 408–424. Elsevier BV.
Download: PDF published in NeuroImage – DOI
Abstract
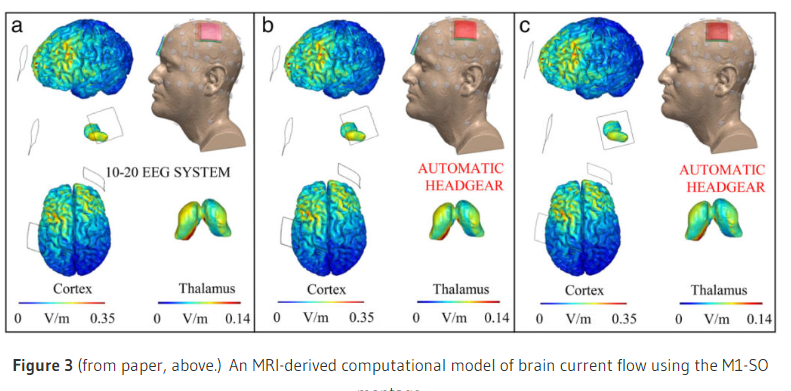
Online imaging and neuromodulation is invalid if stimulation distorts measurements beyond the point of accurate measurement. In theory, combining transcranial Direct Current Stimulation (tDCS) with electroencephalography (EEG) is compelling, as both use non-invasive electrodes and image-guided dose can be informed by the reciprocity principle. To distinguish real changes in EEG from stimulation artifacts, prior studies applied conventional signal processing techniques (e.g. high-pass filtering, ICA). Here, we address the assumptions underlying the suitability of these approaches. We distinguish physiological artifacts – defined as artifacts resulting from interactions between the stimulation induced voltage and the body and so inherent regardless of tDCS or EEG hardware performance – from methodology-related artifacts – arising from non-ideal experimental conditions or non-ideal stimulation and recording equipment performance. Critically, we identify inherent physiological artifacts which are present in all online EEG-tDCS: 1) cardiac distortion and 2) ocular motor distortion. In conjunction, non-inherent physiological artifacts which can be minimized in most experimental conditions include: 1) motion and 2) myogenic distortion. Artifact dynamics were analyzed for varying stimulation parameters (montage, polarity, current) and stimulation hardware. Together with concurrent physiological monitoring (ECG, respiration, ocular, EMG, head motion), and current flow modeling, each physiological artifact was explained by biological source-specific body impedance changes, leading to incremental changes in scalp DC voltage that are significantly larger than real neural signals. Because these artifacts modulate the DC voltage and scale with applied current, they are dose specific such that their contamination cannot be accounted for by conventional experimental controls (e.g. differing stimulation montage or current as a control). Moreover, because the EEG artifacts introduced by physiologic processes during tDCS are high dimensional (as indicated by Generalized Singular Value Decomposition- GSVD), non-stationary, and overlap highly with neurogenic frequencies, these artifacts cannot be easily removed with conventional signal processing techniques. Spatial filtering techniques (GSVD) suggest that the removal of physiological artifacts would significantly degrade signal integrity. Physiological artifacts, as defined here, would emerge only during tDCS, thus processing techniques typically applied to EEG in the absence of tDCS would not be suitable for artifact removal during tDCS. All concurrent EEG-tDCS must account for physiological artifacts that are a) present regardless of equipment used, and b) broadband and confound a broad range of experiments (e.g. oscillatory activity and event related potentials). Removal of these artifacts requires the recognition of their non-stationary, physiology-specific dynamics, and individualized nature. We present a broad taxonomy of artifacts (non/stimulation related), and suggest possible approaches and challenges to denoising online EEG-tDCS stimulation artifacts.